
A conversation with Novo Nordisk
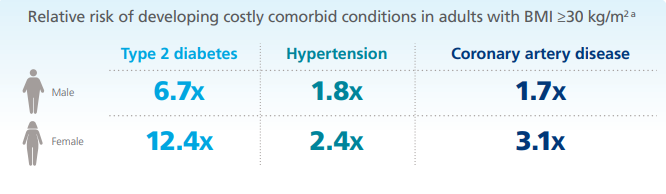
Michigan is consistently ranked among the top 10 to 15 most obese states in the United States. More specifically, 35.2% of adults in Michigan are obese, while 34.6% are considered overweight, according to a 2020 Michigan Behavioral Risk Factor Survey. Obesity increases the risk of developing severe chronic health conditions, including type 2 diabetes, hypertension, and coronary artery disease.
The prevalence of obesity across the United States continues to increase. If the current trend continues, 51% of the U.S. adult population will have obesity by 2030.
Employers should have a vested interest in supporting employees who are obese or overweight on their weight loss journey as a benefit to employee mental health and quality of life, company performance, and annual health care costs.
The Pandemic and Obesity Rates
Adults with excess weight are at a greater risk of severe COVID-19 illness, according to the Centers for Disease Control and Prevention (CDC). Obesity may triple the risk of hospitalization because of COVID-19 infection. The higher an individual’s BMI, the greater risk of hospitalization, admission to an intensive care unit, oxygen, invasive mechanical intervention, and death.
Due to various psychological factors, including isolation, anxiety, and stress, obesity rates across the U.S. increased throughout the pandemic. According to a 2021 American Psychological Association study, 42% of U.S. adults reported an undesired weight gain since the start of the pandemic, with an average weight gain of 29 lbs. From a public health perspective, this is especially concerning, knowing that obesity is an underlying condition for a variety of chronic health conditions and severe COVID-19 illness.
Obesity Disproportionately Impacts Some Racial and Ethnic Minority Groups
Data gathered by the CDC from 2018-2020 found that Hispanic and non-Hispanic Black adults have a higher prevalence of obesity and are more likely to suffer worse outcomes from COVID-19. Racial and ethnic minority groups have historically had fewer opportunities for economic, physical, and emotional health, and these inequities have increased the risk of COVID-19 illness and death for some populations.
Obesity Stigma Explained
Negative attitudes toward individuals who are obese are widely integrated and accepted in North American society. Studies have documented harmful weight-based stereotypes that overweight and obese individuals are weak-willed, noncompliant, and unsuccessful with weight-loss treatment. Stereotypes like these contribute to stigma and discrimination against individuals who are obese in all areas of life, including the workplace, health care facilities, education systems, media, and close personal relationships.
Obesity stigma threatens health, generates health disparities, and interferes with effective obesity intervention efforts. Unfortunately, as a society, we lack the understanding, mindset, and empathy to see obesity as the disease it is.
Employers, payers, health systems, coalitions, affiliations, and chambers must collectively recognize obesity as a disease to achieve better health outcomes in Michigan.
The Link Between Obesity and Mental Health
There is a strong correlation between obesity and negative mental health outcomes. For example, a recent study found that adults with excess weight had a 55% higher risk of developing depression over their lifetime than individuals who did not experience challenges with maintaining a healthy weight. Additional research linked being overweight with major depression, bipolar disorder, and panic disorder.
It should be noted the link between obesity and mental health goes both ways. Poor mental health conditions can lead to obesity through several behaviors including:
- Chronic stress, anxiety, and depression may cause individuals to use food as a coping strategy.
- People with serotonin deficiency may self-medicate with food because carbohydrate cravings increase depressed mood, interrupted sleep patterns, and anxiety.
- Individuals who are depressed may lack the energy or desire to exercise or participate in other activities they usually enjoy.
What if we called obesity something different?
By simply reversing the spelling of obesity to “Ytisebo,” an experiment conducted by Novo Nordisk illustrates the negative stigma associated with the disease:
After reading a commercial script with statistics about a disease called “Ytisebo,” participants learn that the prompt is about obesity. “Is this a joke?” asked one participant. A range of emotions overwhelm participants, including embarrassment, shock, and empathy.
“I didn’t realize it was so serious,” said one participant.
“It’s funny because we just judge without even thinking about it,” another said.
“It’s more than just diet and exercise. It’s a really serious disease. I’m sorry guys,” said another.
The Impact of Obesity in the Workplace
Financially, the impact of obesity on employers is significant:

Obesity may be contributing to other costs. According to a study, obesity-related health complications cost employers:
- $111.9 billion due to type 2 diabetes
- $42.1 billion due to osteoarthritis
- $10.9 billion due to coronary heart disease
Obesity among the workforce doesn’t only impact employer health plan costs but also imposes adverse effects on operations and culture.
Obesity may cause employees to miss more workdays. In a study referencing 2006-2008 survey data, employees with a BMI of 40 kg/m will miss 77% more workdays than those with a BMI of 25 kg/m. Additionally, the study found that obesity-related absenteeism can cost employers $12.8 billion annually.
Obesity is also associated with increased presenteeism. Presenteeism is the average amount of time between arriving at work and starting work on days when an employee is not feeling well and the average frequency with which an employee:
- Loses concentration
- Feels fatigued at work
- Works slower than usual
- Does nothing at work

The Employer’s Role
Many employers already have wellness programs and health plans in place, but most efforts don’t recognize obesity as a disease.
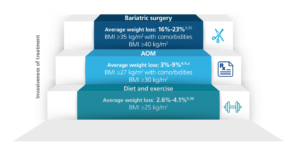
Many employers encourage staff to lose weight through lifestyle changes with fun challenges for walking and nutrition; however, there is a significant gap in employer support between fun challenges and extreme bariatric surgery. In most cases, there isn’t much to provide effective support and avoid surgery altogether.
One strategy for addressing the obesity care gap is considering coverage for anti-obesity medications (AOMs) as a treatment option through the company health plan.
Add Weight Management Support to Employee Benefits
AOMs are noninvasive, FDA-approved therapies that can benefit those with a BMI ≥27 kg/m2 and weight-related comorbidities or a BMI ≥30 kg/m2 as an adjunct to lifestyle modification.
Adding AOMs to employee benefits offerings may support employees with obesity. Even a 5- 10% weight loss can help employers reduce annual medical costs.
For more information and studies on the benefits of including AOMs in employee benefits offerings, visit Novo Nordisk Works and Recognize the Impact, The Weigh Forward.