
To achieve better health outcomes in southeast Michigan, employers must commit to helping employees eliminate barriers to quality health care. Promoting health equity in the workplace can reduce health care costs while improving employee health and productivity.
At the Detroit Regional Chamber’s Employer Forum: The Business Case for Employee Health Equity hosted in partnership with Blue Cross Blue Shield of Michigan (BCBSM) on Thursday, Nov. 3, attendees heard strategies from Bridget Hurd, vice president of inclusion and diversity at BCBSM, about creating equitable workplaces and supporting employees.
Presentation Slides
Key points
- Employers have a responsibility to their workforce and community to help employees access quality health care.
- Health and health care disparities cost $93 billion in excess health care costs and $42 billion in lost productivity.
- It takes a village to make effective, systemic, and community-focused changes toward advancing health equity.
- Eighty percent of health outcomes are determined by an individual’s physical environment, social determinants, and behavioral factors.
- Socially informed screening questions conducted annually can help employers identify inequities among their employee population.
What is Health Equity?
According to the Robert Wood Johnson Foundation, “health equity means that everyone has a fair and just opportunity to be as healthy as possible.”
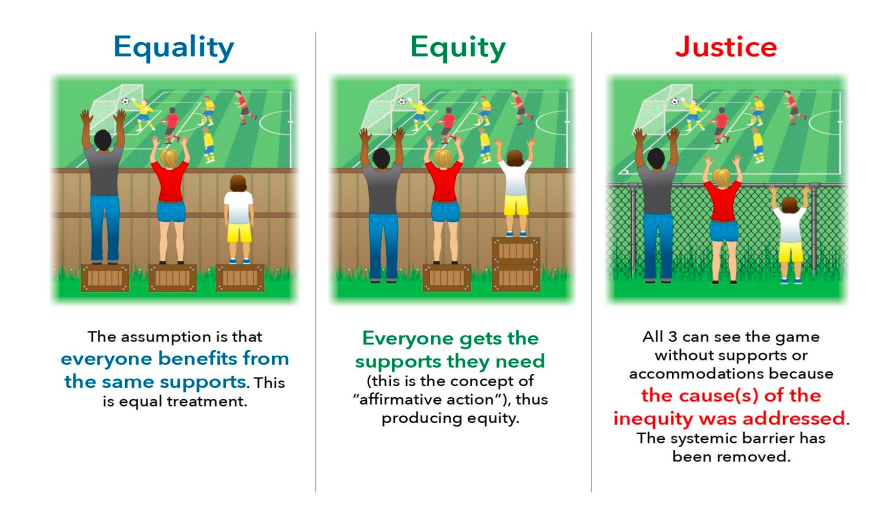
One size does not fit all, especially when it comes to health outcomes. Health equity is the opportunity for every individual to receive optimal care for their specific needs.
“Over time, especially in recent years, we need to pay attention to how people live and the difference exposures people have in their environment,” said Hurd. Doing so can help employers better understand the unique challenges employees are facing.

Social Justice
With social justice comes the opportunity to evaluate and address policies and processes to better support employee health.
“So often, we assume that because someone carries an insurance card, they have equal access to all health benefits, but that’s not the case,” said Hurd.
According to the Robert Wood Johnson Foundation, “[social justice] requires removing obstacles to health such as poverty, discrimination, and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education, and housing, safe environments, and health care.”
Social Inequities Contribute to Poor Health Outcomes
A few examples in recent years:
- People in lower-income households are at higher risk of serious illness if infected with Coronavirus.
- People of color face longstanding disparities in health coverage.
- The median net worth of White households is 11 times that of Black households.
“Plenty of research proves bias in healthcare based on generations and generations of thoughts that have been passed down,” said Hurd.
Therefore, it takes a village to make effective, systemic, and community-focused changes toward advancing health equity. Employers are just one piece of this effort – commitment toward improving health equity is also needed from policymakers, providers, health plans, and communities.
The COVID-19 pandemic shed light on how social determinants, health disparities, and health care disparities can impose dangerous challenges. For example, in the early months of the pandemic, African American and Black residents, as well as Native American, Hispanic/Latino, and people with disabilities, faced many barriers, including access to testing sites, unconscious bias at testing sites, being frontline workers, food insecurity, underlying health conditions where disparities are already prevalent, such as obesity, diabetes, and other conditions.
For women, maternal deaths rose significantly during the first year of the pandemic, especially among Black and Hispanic women. One-third of pregnant women and new mothers who died in 2020 were Black, despite Black Americans making up 13% of the population. Moreover, the mortality rate among Black women was nearly three times that of White women.
Additionally, members of the LGBTQ+ community encounter many disparities, challenges, and barriers in health care.
- LGBTQ+ youth are 120% more likely to experience homelessness than non-LGBTQ youth.
- 17% of LGBTQ+ adults do not have any kind of health insurance coverage, compared to 12% of non-LGBTQ+ adults.
- In Michigan, 25% of LGBTQ adults experience food insecurity, compared to 15% of non-LGBTQ+ adults.
“The light was shining on something we’ve known but had not taken action on,” said Hurd.
Health Disparities vs. Health Care Disparities – What’s the Difference?
Health disparities revolve around illness, injury, disability, and mortality. Health care disparities reference differences in health insurance coverage and access to care, including utilization of care and quality of the care provided.
Health and health care disparities are often viewed through the lens of race and ethnicity, but they occur across a broad range of dimensions:
- Socioeconomic status
- Gender
- Age
- Geography
- Language
- Citizenship status
- Disability status
- Sexual identity and orientation
Health and health care disparities greatly impact the workplace, costing $93 billion in excess health care costs and $42 billion in lost productivity.
“This is an opportunity for employers to work directly with their health plan to identify disparities and work on programming together,” said Hurd. Questions for consideration may include:
- Are there care gaps in our company health plan?
- What barriers might exist for employees to access care?
- Is everyone being represented and having an opportunity to receive care?
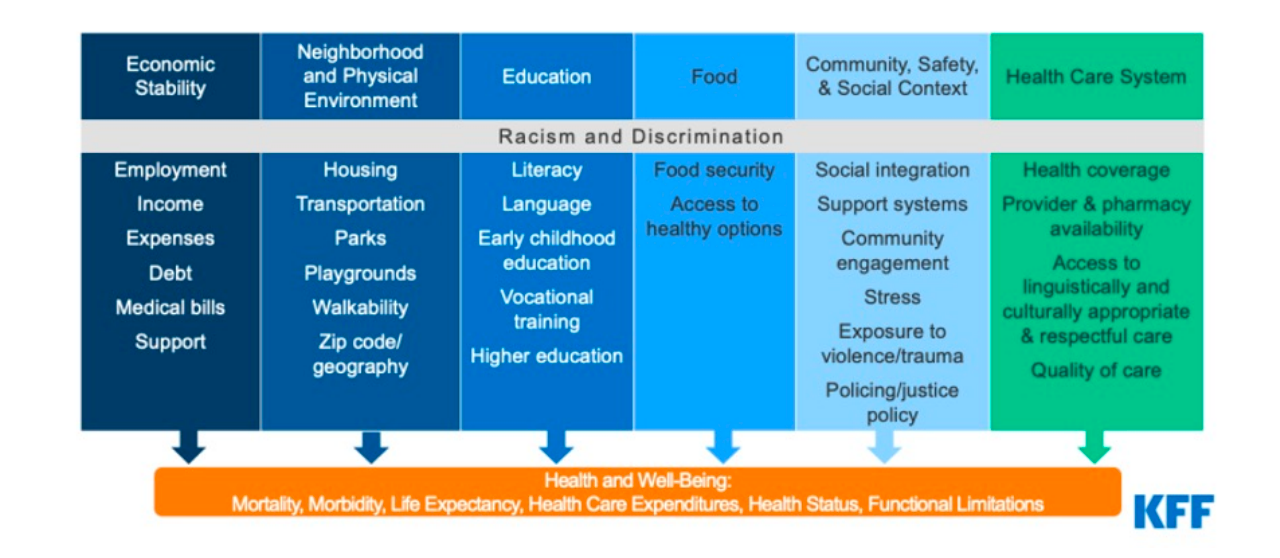
Social Determinants
Social determinants of health are circumstances in which people are born, grow up, live, work, and age, and the systems put in place to deliver health care. These factors matter because 80% of health outcomes are determined by an individual’s physical environment, social determinants, and behavioral factors, meaning a mere 20% of a person’s health and well-being are tied to their medical care.
“Our health is not solely impacted by conversations at the doctor’s office,” said Hurd.
Six categories of social determinants of health:
The Business Case for Advancing Health Equity in the Workplace
What employers can do:
- Provide employer-sponsored health insurance.
- Regularly evaluate health benefits and services, especially concerning behavioral health and needs of LGBTQ and people with disabilities.
- Understand health and health care disparities among the employee population.
- Understand and address social determinants of health.
- Identify health care equity barriers for employees.
- Expand benefits to help employees meet basic needs, such as housing and transportation.
- Ensure benefits are easy to access and understand.
- Bring health screenings, health coaches, and other services directly to the worksite.
- Change workforce culture to destigmatize receiving care and focus on wellness and prevention.
- Partner with other organizations and be a voice for your employees.
Socially informed screening questions conducted annually can help employers identify inequities among their employee population. However, don’t make assumptions about their barriers – employers should ask, listen, and remember that one size does not fit all. Some questions can include:
- What services do you need more convenient or affordable access to?
- Do you have immediate concerns about your housing, transportation, or personal safety?
- Other questions related to food security, childcare, health care quality, education, utilities, and financial strain.
Employers have the power to make a positive impact on the health of their employees. The first step is committing to address health disparities. Then start the conversation to understand employees’ unique needs.
Reminders:
- Employers conduct these assessments annually. “Things change in people’s lives,” said Hurd. “Annual assessments will help inform where you should pivot on the work you may already be doing.”
- Explain the why – don’t just send the survey. Clearly explain why leadership is interested in better understanding health, health care, and its disparities. Get as specific as possible.
- Communication is key to helping employees feel safe and secure. Help employees feel comfortable answering honestly by ensuring the survey responses are anonymous.
Resources for developing screening questions:
“Health equity is not a special project – health equity should be embedded into everything and all actions we take,” said Hurd. “It’s hard work, the change is not always immediate, but in terms of connecting people to resources and ensuring better understanding of health coverage, employers can support employees and minimize stigma.”