You may have heard concerns of a disease called Monkeypox that was recently declared a public health emergency by the World Health Organization, the U.S. Department of Health and Human Services, and some states and localities. As Monkeypox circulates in Michigan, many are experiencing resurfacing feelings of fear, stress, and anxiety brought on by the news of the COVID-19 pandemic in 2020. According to experts, there are 73 cases of Monkeypox in Michigan as of August 10, 2022. Below are answers to common questions and guidance from public health experts as Michigan navigates the outbreak.
What is Monkeypox?
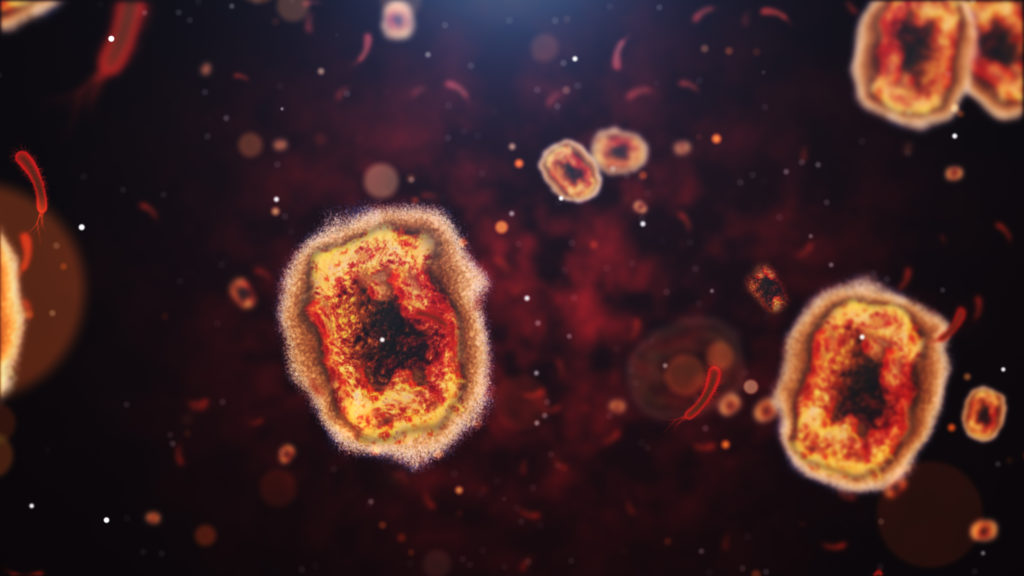
Monkeypox is a rare disease caused by infection with the monkeypox virus. The virus is part of the same family of viruses as variola virus, the virus that causes smallpox. Monkeypox was discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research. The source of the disease remains unknown, however, it is believed African rodents and non-human primates (like monkeys) might harbor the virus and infect people, according to the Centers for Disease Control and Prevention (CDC).
Prior to the current outbreak, monkeypox had been reported in people in several central and western African countries. Previously, almost all monkeypox cases were linked to international travel to countries where the disease commonly occurs or through imported animals.
How does Monkeypox spread?
“This virus is spread through very close contact, often skin to skin. Monkeypox causes lesions and rashes, and the fluid from the lesions and rashes are infectious. It also can be through droplets, that is, droplets that are released through your mouth, through even just talking. The virus can, in addition, contaminate objects like fabrics and it can survive there for a period of time, and people can be exposed through touching those objects, but this mode of transmission seems to be rare,” said Joseph Eisenberg, epidemiologist at the University of Michigan School of Public Health in a recent article.
Monkeypox does not spread like COVID-19. While public health experts recognize the Monkeypox outbreak as a global pandemic, it will not spread as rapidly as COVID-19. “First of all, it can’t aerosolize into the air and therefore stay in the air for hours or even days like COVID. Second of all, it requires a much higher dose to become infected. So, the fact that it’s much less infectious is one reason why monkeypox will not spread in the way we see something like COVID spreading,” said Eisenberg.
Symptoms
Common Monkeypox symptoms include a rash that may be located on the hands, feet, chest, face, or mouth as well as on or near the genitals or anus.
- The rash will go through several stages, including scabs, before healing.
- The rash can initially look like pimples or blisters and may be painful or itchy.
Other symptoms of monkeypox can include:
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
Some may experience all or only a few symptoms. Sometimes, people have flu-like symptoms before the rash. Some people get a rash first, followed by other symptoms. Others only experience a rash.
Monkeypox symptoms usually start within 3 weeks of exposure. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later. The individual is contagious from the time symptoms start until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed. On average, the illness typically lasts 2-4 weeks.
People experiencing monkeypox symptoms or have had close personal contact with someone who has the disease should visit a healthcare provider who can assess whether they should be tested.
How dangerous is Monkeypox?
While similar to smallpox symptoms, Monkeypox symptoms are milder and rarely fatal, according to the CDC.
Over 99% of people who contract the West Africa Type form of the disease are likely to survive. However, people with weakened immune systems, children under 8 years of age, people with a history of eczema, and people who are pregnant or breastfeeding may be more likely to get seriously ill or die.
The Congo Basin type of monkeypox virus has a fatality rate around 10%.
Is there a Monkeypox vaccine?
Yes, a Monkeypox vaccine was issued an emergency use authorization by the U.S. Food and Drug Administration on August 9, 2022 for the JYNNEOS vaccine. Healthcare providers are permitted to use the vaccine for individuals 18 years of age and older who are determined to be at high risk for monkeypox infection. JYNNEOS, the Modified Vaccinia Ankara (MVA) vaccine, was approved in 2019 for prevention of smallpox and monkeypox disease. To learn more about the development of this vaccine and eligibility, visit FDA.gov.
How can risk of monkeypox be minimized?
- Avoid close, skin-to-skin contact with people who have a rash that looks like monkeypox.
- Avoid contact with objects and materials that a person with monkeypox has used.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.
- If you plan to attend an event, consider how much close, personal, skin-to-skin contact is likely to occur there.
With any disease outbreak, it is important to assess your current risk level and consider temporary lifestyle changes for prevention.
For additional information, please visit 5 Facts You Need to Know About Monkeypox.